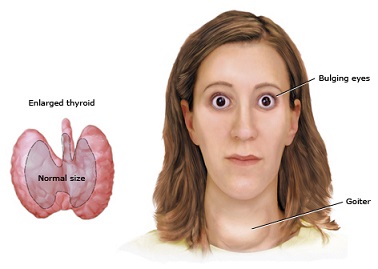
Thyrotoxicosis or hyperthyroidism is relatively rare in children. According to reports, the yearly incidence is 8 per 1 million children who are younger than 15 years old and 1 per 1 million in children younger than 4 years old. Among these patients, Graves’ Disease is the most common cause. It is noted that girls are affected five times more than boys. A family history of hyperthyroidism should be sought because many have a positive family history of autoimmune thyroid diseases. A clinical profile includes several month records of progressive symptoms, of which, the most common are often behavioral disturbances such as decreased attention span, difficulty concentrating, emotional liability, hyperactivity, difficulty sleeping, and nervousness. On examination by a doctor, an enlarged thyroid gland is usually palpated in the majority of cases. The thyroid gland is characterized by a diffuse enlargement which is smooth, firm and nontender.
When thyroid disease is considered based on the symptoms and physical examination findings, further diagnostic examination should be done to confirm the diagnosis. This includes getting a blood test to check for thyroid hormones and a thyroid ultrasound to examine the characteristics of the thyroid gland.
Once confirmed, management can include one or more of the following:
- Antithyroid medications such as methimazole or propylthiouracil (PTU)
- Radioactive iodine therapy
- Thyroidectomy
Antithyroid drugs are given to inhibit thyroid hormone synthesis as well as the peripheral conversion of thyroxine, the inactive thyroid hormone to the more active thyroid hormone, triiodothyronine.
Among the abovementioned antithyroid drugs, methimazole is the preferred drug for use in children. However, one should be cautious as these antithyroid medications are not free from side effect. In fact, side effects from these medications can be life-threatening. More common side effects include allergic reactions, hypothyroidism from overtreatment, and agranulocytosis which can lead to severe sequelae. Data on the prevalence of agranulocytosis in children are unavailable, but is estimated to be very low. Persistent minor cutaneous allergic reactions are usually managed by concurrent antihistamine treatment or cessation of the medication, but it should definitely be the managing doctor’s decision.
Vasculitis is a rare complication during treatment of thyrotoxicosis in children. Affected organ systems have been primarily renal, musculoskeletal, and dermatologic. The first case of thionamide-induced central nervous system vasculitis was reported in 2005 which presented with confusion and later on resolved upon discontinuation of the drug. Although cerebral involvement is seldom observed with PTU treatment, cerebral vasculitis should be considered in patients developing CNS symptoms. Despite accumulating reports demonstrating ANCA associated vasculitis following treatment with antithyroid drugs, most ANCA positive patients do not have manifestations of vasculitis.
PTU was responsible in 93% of cases of thionamide-induced ANCA-positive vasculitis. It has been discovered in studies that the drug accumulates in the neutrophils, a type of white blood cell and it results to changes in the cell’s structure making it susceptible to triggering an immunologic response by the body.
In patients who cannot tolerate antithyroid medications, such as those that develop serious side effects from the medications, either radioactive iodine therapy or surgery is considered.
Other symptomatic treatment includes giving medicine to control the heart rate. This includes giving a beta-blocker such as propranolol. This is recommended especially for children experiencing symptoms of hyperthyroidism especially those with heart rates over 100 beats per minute.
Upon starting antithyroid medications, monitoring of response to therapy should be done. Blood tests that include thyroid function tests are obtained monthly at first, and then every 2 to 4 months. Immunologic markers such as TrAb is sometimes done in patients suspected of having an immunologic cause for their thyroid dysfunction. If this is done, studies show that its level normalizes after 24 months in only 18% of pediatric patients.
Lasting remission after antithyroid drug therapy occurs only in a small minority of pediatric patients. When antithyroid drugs are used for 1-2 years, remission rates are generally 20 to 30%, with remission being defined as having normal thyroid function test for 1 year after cessation of therapy. If remission is not achieved after a course of treatment with antithyroid drug treatment, radioactive iodine therapy or surgery should be considered next.

 (9 votes, average: 4.56 out of 5)
(9 votes, average: 4.56 out of 5)