By:
Christine Rhea S. Igna, MD*
Jesus A. Relos, MD**
Abstract
Objective: To present a case of multiple myeloma who developed osteonecrosis as one of the complications of bisphosphonate therapy.
Setting: University of Perpetual Help DALTA Medical Center
Case Summary: This is a case of a 59 year-old female was seen due to pain and purulentdischarge on the right mandible. Patient is a diagnosed case of multiple myeloma three years prior to admission who was treated with melphalan, prednisone, zolendronic acid, and has undergone radiotherapy for 25 sessions. Panoramic radiograph of the mandibles showed radioluscency at the body of mandible suggestive of an osteonecrotic process. After discovering this, zolendronic acid was discontinued and sequestrectomy and hyperbaric oxygen was done as advised by the maxillofacial surgeon.
Keywords: multiple myeloma; osteonecrosis
Introduction
Multiple myeloma is a hematologic malignancy characterized by the clonal expansion of malignant plasma cells within the bone marrow. Plasma cells are antibody-(immunoglobulin-) producing cells. When these cells grow out of control, they crowd out normal blood forming cells which eventually invades the osseous system. Myeloma-related lytic bony disease is now understood to be secondary to increased osteoclastic activity and impaired osteoblastic activity.
Despite the proven benefits of bisphosphonates in patients with multiple myeloma, the mechanism of bisphosphonates-induced osteonecrosis remains unclear. The following predisposing factors were identified: immunocompromised state which increases the risk to various infections, corticosteroid use, history of trauma; vascular insufficiency and a hypercoagulable state.1
Osteonecrosis of the jaw is one of the recently described adverse effects of bisphosphonate therapy. The mandible is more commonly affected than the maxilla (2:1 ratio).2 Those with multiple myeloma and bone metastasis who are receiving intravenous, nitrogen-containing bisphosphonates are at greatest risk for osteonecrosis of the jaws; these patients represent 94% of published cases and 60% of cases are preceded by a dental surgical procedure.5
This case report describes one of the complications of bisphosphonates in a multiple myeloma patient who has shown to be compliant to chemotherapy, radiotherapy and supportive care.
Case Report
This is a case of a 59 year-old female who was diagnosed to have multiple myeloma three years prior to admission. Her initial presentation was a persistent low back pain,which on further diagnostic workup revealed her condition. She was thereby advised to have radiation therapy and was placed on oral chemotherapy with melphalan and prednisone. Two years prior to admission, after seven sessions of radiotherapy, patient complained of headache, characterized as throbbing at the left temporo-parietal area, associated with pain and blurring of vision of the left eye. Her blood pressure was 140/90 mmHg. Cranial CT scan was done, which showed bony lytic changes in the base of the skull and an opacified left sphenoid sinus compatible with sinusitis. She was treated for sinusitis and was given antibiotics. She was also started on monthly intravenous zolendronic acid. She was discharged improved. The patient was maintained on melphalan, dexamethasone (six months) andzolendronic acid (one year). One year prior to admission, patient complained of pain of the right jaw initially mistaken for dental caries. However, there was noted progression of swelling and purulent dishcharge on the right body of the mandible. The patient sought consult with a maxillofacial surgeon to which a panoramic and periapicalxray were done that revealed a radioluscent area, approximately 2.5 x 3.5 cm with no clear border, periapical to tooth 45 extending to the posterior area at medial aspect of the roots of tooth 67 (Figure 1). Bone scintigraphy was also done which showed multiple activity of widespread osseous metastasis and increased bone turn over in the body and ramus of the manbible(Figure 2). All the radiographic data and clinical presentation described are compatible to osteonecrosis of the bone Stage II (based from Table I) attributed to be secondary to bisphosphonates. Hyperbaric oxygen therapy, antibiotic prophylaxis and sequestrectomy was done. Histopathology showed diffuse coagulative necrosis which is compatible with osteonecrosis. The monthly treatment of intravenous zolendronic acid was resumed after three weeks.
Discussion
The use of bisphosphonates is one of the mainstay of treatment of patients with multiple myeloma bony related disease. However, despite the benefits of minimizing the complications and metastatic progression, it has shown that the occurrence of osteonecrosis of the jaw of nine point five fold with zolendronic acid to which 65% is located at the mandible.4,5
The mean time of the onset of ONJ among patients using zolendronic acid is 18 months in comparison with this case of approximately 12 months.6
Since ONJ is one of the threatened complications of bisphosphonate use it has lead to the following 3 H principle of pathophysiologic state: hypocellular, hypovascular and hypoxic tissues. This impedes the replacement of connective tissues and cells as part of tissue turnover in normal homeostasis and in wound healing. Breakdown of tissues can thus ensue with or without trauma. This leads to a problem of impaired and inadequate tissue turnover and wound healing.7
Sequestrectomy and hyberbaric oxygen therapy have been showed to improve the worsening of complications since restores the steep oxygen gradient needed for wound healing. It has been shown that 94.7% of cases showed improvement without experiencing complications of the procedure.7Ibid
Up to this point in time, there are currently no data available to recommend discontinuing, maintaining or temporarily interrupting bisphosphonate therapy once ONJ has developed. As bisphosphonates are not metabolized and continue to maintain high concentrations within bone for long periods of time, it remains unclear if altering the dose, schedule or type of bisphosphonate affects the symptomatic complication rate of ONJ.3
Conclusion and Recommendations
The risks and benefits of bisphoshonates use in patients with multiple myeloma has been emphasized. Education, early detection, and prompt diagnosis are of great concern. Both physicians and patients should be aware of ONJ as a possible complication.2,3
Future research, genomic studies and prospective clinical trials is recommended to explain the pathogenesis of this process and to accurately define the clinical and perhaps genetic risk factors of ONJ in relation to multiple myeloma.1,8
Figures and Table
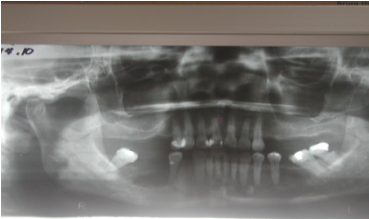 Figure 1. Panoramic Radiograph: A radioluscent area periapical to tooth 45 extending to the posterior area at medial aspect of the roots of tomoth 67 and radioluscency was noted approximately 2.5 X 3.5 cm and has no clear border
Figure 1. Panoramic Radiograph: A radioluscent area periapical to tooth 45 extending to the posterior area at medial aspect of the roots of tomoth 67 and radioluscency was noted approximately 2.5 X 3.5 cm and has no clear border
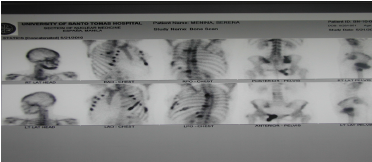
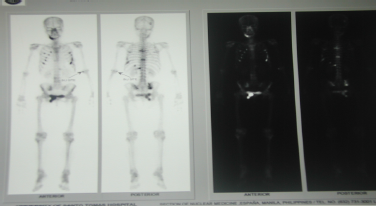 Figure 2. Bone Scintigraphy: Multiple activity of widespread osseous metastasis and increased bone turn over in the body and ramus of the manbible
Figure 2. Bone Scintigraphy: Multiple activity of widespread osseous metastasis and increased bone turn over in the body and ramus of the manbible
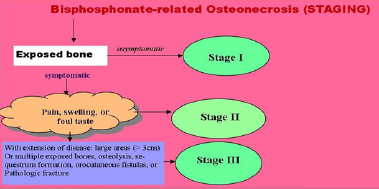 Figure 3. Staging of Bisphosphonate-related Osteonecrosis. Source: New England Journal of Internal Medicine: 1283-1291;358; March 20, 2008
Figure 3. Staging of Bisphosphonate-related Osteonecrosis. Source: New England Journal of Internal Medicine: 1283-1291;358; March 20, 2008
Acknowledgement
The author wishes to thank Vladimir Siangho, MD, Physician and Medical Writer for editing and proofreading the text and figures.
References
1. Tozi, Patrizia, et.al. Osteonecrosis of the jaws in newly diagnosed multiple myeloma patients treated with zoledronic acid and thalidomide-dexamethasone. Blood,Vol. 108, No.12.pp. 3951-3952. December 1, 2006.
2. Roseberg, Andrew, et.al. Case 9-2008: A 65-Year- Old Woman with a Nonhealing Ulcer of the Jaw. New England Journal of Internal Medicine: 1283-1291;358;March 20, 2008
3. Kyle, Robert, et.al. American Society of Clinical Oncology 2007 Clinical Practice Guideline Update on the Role of Bisphosphonatesin Multiple Myeloma. Journal of Clinical Oncology, Vol. 25 No. 17.pp. 2452-2472. June 10, 2007
4. Brufsky, Adam, et.al. Bisphosphonates: Rationale for Use as Adjuvant Therapy. Clinical Care Options: Oncology. pp 5-13. 2009
5. Mehrotra,Bhoomi & Salvator Ruggiero. Bisphosphonate Complications Including Osteonecrosis of the Jaw. American Society of Hematology.pp 356-360. 2006.
6. Ruggiero,Sl. Guidelines for the diagnosis of bisphosphonate related osteonecrosis of the jaw (BRONJ). Clinical Cases in Mineral and Bone Metabolism; 4(1): 37-42. 2007
7. David, Leslie et.al. Hyperbaric Oxygen Therapy and MandibularOsteoradionecrosis: A Retrospective Study and Analysis of Treatment Outcomes. Journal of the Canadian Dental Association Vol. 67, No. 7.pp 384-390. July/August 2001.
8. Smith, Alla, et.al. Oral Osteonecrosis Associated with the Use of Zoledronic Acid: First Case of a Patient with Advanced Pancreatic Cancer and Bone Metastases. Journal of the Pancreas. Vol 10 No 2. pp. 212-214. March 9, 2009.
* Resident, Physician Internal Medicine University of Perpetual Help DALTA Medical Center (UPHDMC)
**Internist-Hematologist, UPHDMC, Makati Medical Center, St. Dominic Medical Center, AHMC .
Not only do both team members need to be competent writers https://www.affordable-papers.net/ who can present ideas in an interesting manner to the reader, they also need to be professional researchers who know where to get the most dependable sources of advice and where to avoid them.

 (6 votes, average: 4.33 out of 5)
(6 votes, average: 4.33 out of 5)